What is a hiatal hernia?
I remember hearing the words “hiatal hernia” for the first time and having absolutely no idea what it meant. All I knew was that something wasn’t right with my digestion—I was feeling uncomfortable, bloated, and dealing with that annoying burning in my chest way too often.
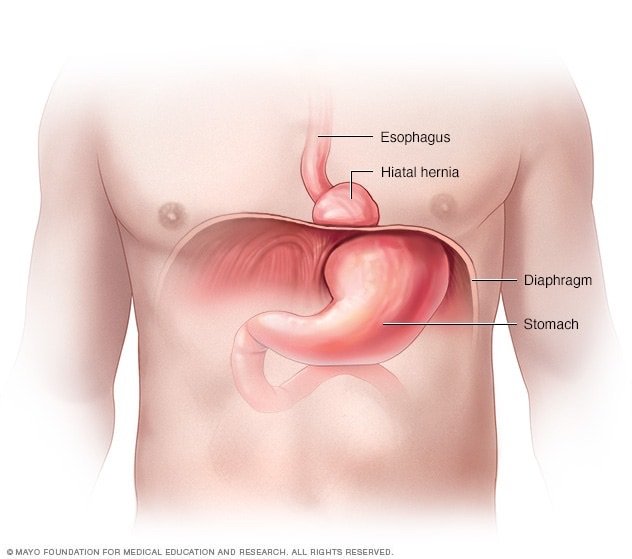
A hiatal hernia happens when part of your stomach pushes up through the diaphragm and into your chest. Your diaphragm is that thin muscle that helps you breathe and separates your stomach from your chest. There’s a small opening in it called the hiatus, and when the upper part of your stomach slides or pushes through that space, that’s when a hiatal hernia forms.
Not all hiatal hernias are the same, though. And knowing which type you have makes a big difference when it comes to symptoms, risks, and treatments. That’s exactly why I wanted to break this down in a way that’s easy to understand—because trust me, it’s confusing when you’re trying to figure it out alone.
Why it’s important to understand the different hiatal hernia types
When I was first diagnosed, no one really explained the type of hernia I had—they just gave me a name and a list of pills. But learning the difference between a sliding hiatal hernia, a rolling (paraesophageal) hernia, and a mixed typecompletely changed how I approached my health.
Each type of hiatal hernia affects your body differently. Some are more common and mild, while others can cause serious problems if ignored. Here’s why knowing your specific type matters:
Understanding your hernia type helps you:
- Spot the right symptoms earlier
- Know when lifestyle changes will help—and when surgery might be needed
- Reduce complications like strangulation or chronic acid reflux
- Feel more in control instead of overwhelmed
In this article, I’ll break down Type 1, 2, and 3 hiatal hernias in plain terms—what they are, how they feel, and what you can actually do about them. Because if you’re anything like me, you’re tired of Googling and still feeling confused. Let’s make it make sense.
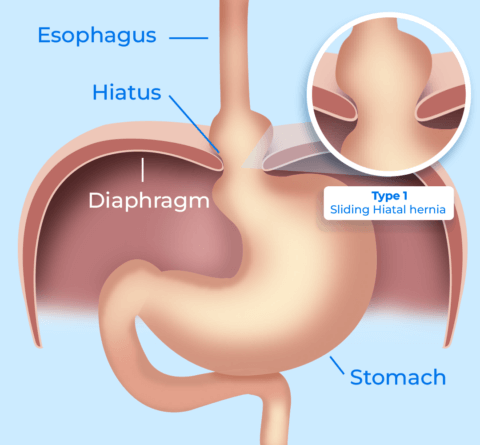
Type 1: Sliding hiatal hernia (the most common one)
This was the type I was diagnosed with—and it’s also the most common kind of hiatal hernia out there. In a sliding hiatal hernia, both your lower esophageal sphincter (LES) and the upper part of your stomach slide up into your chest through the diaphragm. This sliding action can come and go, depending on things like your posture, what you eat, or how full your stomach is.
What it feels like:
- Frequent heartburn or acid reflux
- A sour taste in your mouth
- Trouble swallowing
- Chest pain, especially after meals
- A feeling of fullness, even with small portions
In my case, I kept brushing it off as just “normal” indigestion. But once I understood that the acid reflux was being caused by my stomach literally sliding into my chest, it all made more sense.
If you’re regularly feeling this kind of discomfort, I really recommend reading up on the natural remedies that helped me with heartburn—some of them worked better than meds for me.
How it’s treated:
- Lifestyle changes (smaller meals, weight loss, elevated sleeping)
- Medications like antacids, H2 blockers, or proton pump inhibitors
- Surgery is rare unless symptoms are severe or complications arise
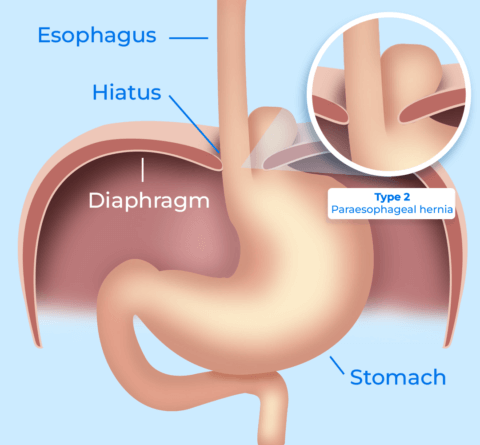
Type 2: Rolling (paraesophageal) hiatal hernia
This one’s much less common—but it’s also a bit more serious. A rolling hiatal hernia, also called a paraesophageal hernia, happens when part of your stomach rolls up next to your esophagus, while the lower esophageal sphincter stays in its normal place.
What makes it different:
- You might not feel reflux—but you can still have major symptoms
- There’s a higher risk of your stomach getting pinched or strangled, which can lead to serious complications if ignored
Common symptoms:
- Chest pressure or pain (not always linked to meals)
- Feeling like food is stuck
- Shortness of breath after eating
- Sometimes no symptoms at all—until it becomes urgent
If you’ve been experiencing strange chest pain and no heartburn, this type of hernia might be the reason. These can sneak up on people and aren’t always easy to spot, so knowing the signs is huge.
One of the biggest risk factors for hernias like this? Chronic pressure on your abdomen, often due to things like coughing, straining during bowel movements, or even being overweight. If that sounds familiar, this guide on gut-friendly lifestyle changes could help reduce that pressure naturally.
In the next section, we’ll cover the most complicated kind—Type 3 mixed hernias, which combine the worst of both types.
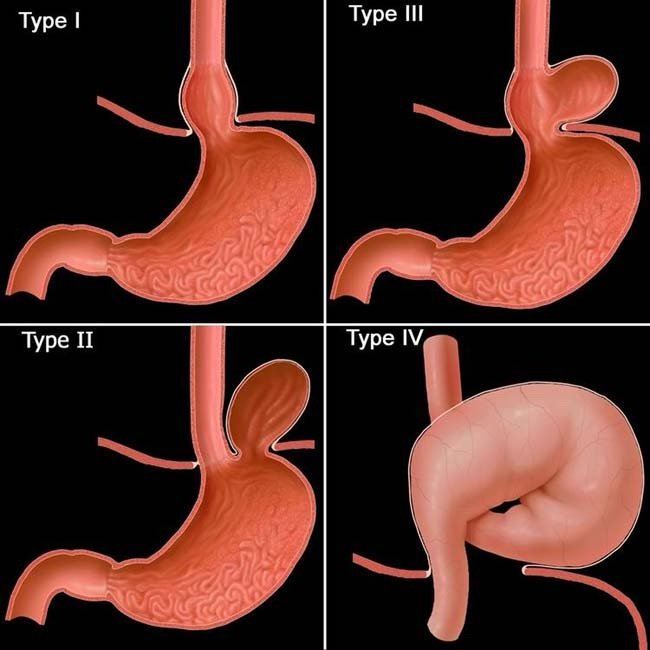
Type 3: Mixed hiatal hernia (when sliding and rolling collide)
This is the type that had me the most concerned when I first learned about it. A Type 3 hiatal hernia is also called a mixed hernia, because it combines elements of both sliding and rolling hernias. That means both your gastroesophageal junction and part of your stomach move up into your chest—but not in the same way as the others.
So basically, it’s the worst of both worlds. You get the reflux and heartburn issues from the sliding component, plus the risk of strangulation and obstruction from the rolling part.
What makes it stand out:
- Higher risk of complications than Type 1 or 2
- Usually causes a mix of reflux symptoms and more serious pressure or breathing issues
- Can go unnoticed for years—or cause sudden, severe symptoms
What I’ve seen (and what the research says):
- Many people don’t realize they have this type until they undergo imaging for chest pain or severe reflux
- It can feel like constant indigestion, heaviness in the chest, or trouble catching your breath after eating
- If left untreated, the stomach can become twisted or pinched, which may require emergency surgery
If your symptoms don’t seem to fit just reflux—or your antacids don’t seem to be doing anything—it’s worth asking your doctor about a barium swallow test or endoscopy to check for more complex hernias.
Also, if your symptoms include chronic pain, gurgling at bedtime, or unexplained bloating, check out our post on stomach gurgling at bedtime—these signs could be tied to digestion troubles or hernias that aren’t always obvious.
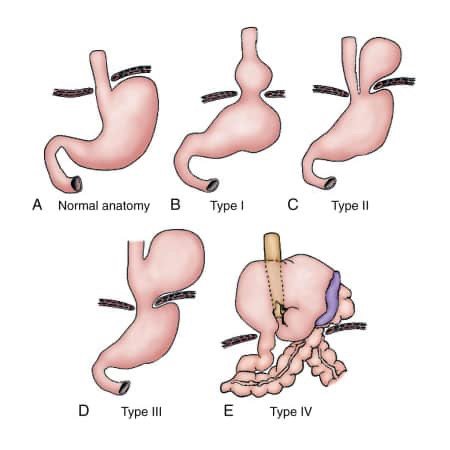
Type 4: The rare but serious one
This one isn’t talked about as much, but it’s worth including. Type 4 hiatal hernias go beyond the stomach and involve other abdominal organs—like your colon, small intestine, or even your spleen—herniating up into the chest cavity.
It’s rare, and often seen in older adults or people who’ve had other types of hernias worsen over time. I personally haven’t experienced this one (and hope I never do), but here’s what I’ve learned from the research:
Signs of a Type 4 hernia:
- Severe chest pain that doesn’t go away
- Difficulty swallowing or keeping food down
- Shortness of breath
- Sudden bloating or fullness
- Vomiting after meals or feeling like food is stuck
This type of hernia almost always requires surgery and shouldn’t be ignored. If you or someone you love is showing these signs, don’t wait—get checked out immediately.
You can help prevent progression of any hernia by supporting your digestion, reducing pressure in the abdomen, and making some consistent lifestyle changes (like the ones I talked about in this guide). Small things really can make a big difference when it comes to prevention.

Common symptoms shared across all hiatal hernia types
What surprised me most when I started learning about the different hiatal hernia types was how much overlap there was in symptoms—even between mild and more serious forms. While the severity and risks can vary, the body often responds in similar ways when your stomach starts slipping out of place.
If you’re wondering whether your symptoms are related to a hiatal hernia, here’s what many of us (myself included) have experienced:
Most common symptoms:
- Heartburn and acid reflux (especially after eating or lying down)
- A burning sensation in your chest or throat
- Bloating and belching
- Difficulty swallowing or a sensation like something is stuck
- Chest pain that may mimic heart-related issues
- Shortness of breath after meals or when reclining
- Regurgitation of food or sour-tasting fluid
- Feeling full after only a few bites
At first, I thought I just had acid reflux, but the deeper I looked, the more I realized that bloating, fatigue, and even shortness of breath after meals were all connected to my hernia. Sometimes these symptoms are mild, but when they start affecting your daily life (or keeping you up at night), it’s time to take them seriously.
If your symptoms seem to get worse when you eat big meals, lie flat after eating, or even just drink water too fast, definitely check out our post on why water can trigger heartburn. That one opened my eyes.
And if your stomach feels worse after pooping or during stressful days, this post on feeling worse after a bowel movement might also help connect some dots.
The takeaway? Hiatal hernias can be sneaky. You might not know what’s happening until symptoms start layering on top of each other. Paying attention to your body’s signals—and getting proper imaging—can help you catch it early and manage it better.

How doctors diagnose the different types of hiatal hernia
I’ll be honest—before getting diagnosed, I didn’t even know what a hiatal hernia was, let alone that there were different types. It wasn’t until I started asking questions and got a proper workup that everything finally made sense.
Getting a solid diagnosis is key because treatment often depends on which type of hernia you’re dealing with. Type 1 might just need lifestyle tweaks and meds, while Type 2 or 3 could require surgical monitoring or even intervention.
Common diagnostic tools doctors use:
- Barium swallow study – You drink a chalky liquid and they take X-rays as it moves through your esophagus and stomach. This was the first test that showed my sliding hernia clearly.
- Upper endoscopy (EGD) – A tiny camera is sent down your throat to look for damage from acid reflux and to check where your stomach is positioned.
- Esophageal manometry – This test checks how well your esophagus muscles work, especially the lower esophageal sphincter (LES), which often gets weak with hernias.
- CT scan or MRI – Sometimes used to look for more complex hernias (like Type 3 or 4) if other tests don’t give clear answers.
If you’re dealing with chronic acid reflux, trouble swallowing, or unexplained chest pressure, push for proper testing. So many people live with a hernia unknowingly—and keep treating symptoms instead of the root cause.
In fact, if your pain seems to move around or flare up during bathroom struggles, it might be worth reading this guide on lower left abdominal pain. Sometimes what feels like a bowel issue can actually be hernia-related.
Getting a clear picture of what’s going on inside your body makes all the difference. Once I saw the X-ray of my stomach pushing upward, I finally understood what was happening—and more importantly, what to do about it.

How each type of hiatal hernia is treated (and what worked for me)
When I first got diagnosed, my mind immediately jumped to surgery. But thankfully, not every hiatal hernia requires an operation. In fact, depending on the type and severity, most people (like me) can manage symptoms and reduce flare-ups with the right combination of lifestyle changes, medication, and knowing what triggers to avoid.
Here’s a breakdown of how treatment usually goes for each type:
Type 1 (Sliding Hiatal Hernia):
This is the most common and often the easiest to treat without surgery.
What usually helps:
- Smaller, more frequent meals to avoid pressure on the stomach
- Elevating your head while sleeping (I stacked pillows for years before switching to a wedge)
- Avoiding trigger foods like acidic tomatoes, coffee, and carbonated drinks
- Medications: antacids, H2 blockers, or proton pump inhibitors (PPIs)
- Natural heartburn remedies also helped me more than I expected
Type 2 (Rolling or Paraesophageal Hiatal Hernia):
These require a bit more monitoring due to the risk of the stomach becoming strangulated.
Treatments may include:
- Watching for signs like severe chest pain or vomiting
- Surgical consultation, especially if symptoms are worsening or if the hernia is large
- Maintaining a healthy weight to reduce internal pressure
- Using natural gut-friendly strategies like these simple lifestyle changes to avoid aggravating the hernia
Type 3 (Mixed Hiatal Hernia):
This is where both sliding and rolling components are involved—so treatment depends on how severe your symptoms are.
What doctors usually recommend:
- Imaging every few years to monitor size and progression
- Managing reflux and pressure symptoms like you would with a sliding hernia
- Surgery if there’s risk of strangulation or if quality of life is declining
Type 4 (Complex Hiatal Hernia):
These usually do require surgery, especially if other organs are involved. The good news is, recovery has come a long way with minimally invasive techniques.
If you’re nervous about the idea of surgery or unsure if you’re at that point, make sure to have a clear conversation with your GI doctor. Ask for a copy of your imaging results so you can actually see what’s going on (that helped me process it way better).
Just remember: a diagnosis doesn’t mean disaster. I’ve been living with a Type 1 sliding hernia for years now, and with the right routine, it barely gets in my way. But when I stray—overeating, skipping sleep, ignoring stress? Yeah… it definitely reminds me who’s boss.

Tips that helped me prevent flare-ups and feel “normal” again
Living with a hiatal hernia doesn’t mean you’re stuck feeling miserable forever. Once I figured out my triggers and developed a routine that worked for me, the heartburn, pressure, and bloating weren’t running my life anymore.
Here’s what made the biggest difference in preventing symptoms—especially with my sliding hiatal hernia:
1. I stopped eating late at night
This one was huge. If I eat within 2–3 hours of bedtime, I almost always feel the burn. Giving my stomach time to empty before lying down cut my nighttime reflux dramatically.
2. I raised the head of my bed
Not just a pillow—my whole upper body. I used a wedge pillow at first, and eventually adjusted my bed frame. It helped keep stomach acid where it belongs. I even noticed my stomach gurgling at bedtime decreased.
3. I simplified my meals
Greasy foods, large portions, or anything carbonated? Guaranteed problems. Now I stick to smaller, balanced meals—especially in the evening. I also added more fiber to help digestion, with things like oats and gut-friendly grains.
4. I started using a probiotic and fiber supplement
They didn’t cure my hernia, but they helped ease bloating and irregularity, which made reflux way less frequent. I found Benefiber with Supergreens especially helpful when my meals lacked variety.
5. I stayed regular
If I got constipated, everything felt worse—pressure, bloating, even chest pain. This gentle stool softener helped me stay on track without harsh side effects, and I’d use Milk of Magnesia on bad days. That routine made a bigger difference than I expected.
If your hernia is affecting how you eat, sleep, or even just go about your day, I promise—it is manageable. But it takes listening to your body and making small changes that actually fit your life. I didn’t fix mine overnight, but with these strategies, I finally felt like myself again.

Know your hernia, know your body
When I was first told I had a hiatal hernia, it felt overwhelming. All I heard was “hernia” and instantly assumed surgery, discomfort, and lifelong issues. But once I took the time to understand the different hiatal hernia types—and how each one shows up in the body—I started feeling more confident and in control.
Whether you’re dealing with a sliding hiatal hernia, a more serious rolling (paraesophageal) hernia, or the combo known as mixed hernia, what matters most is paying attention to your body’s signals and working with—not against—your gut.
Here’s what helped me feel human again:
- Getting a proper diagnosis with a barium swallow and endoscopy
- Building a simple routine using natural remedies for heartburn
- Adding fiber with Benefiber + Supergreens to keep digestion smooth
- Using a stool softener regularly and Milk of Magnesia when needed
- Shifting my focus from “quick fixes” to small lifestyle changes like these 5 that improved my gut health
If you’ve been dealing with reflux, unexplained bloating, chest discomfort, or just that nagging feeling something’s off—it’s worth digging deeper. Understanding your hernia type might be the first step to finally getting relief.
You don’t have to suffer silently. Once I understood what was going on inside my body, everything changed. And with the right approach, you can take your life back—one gut-friendly step at a time.

As an Amazon Associate we earn from qualifying purchases through some links in our articles.