Dealing with Acid Reflux—A Personal Journey
If you’ve ever experienced the discomfort of acid reflux, then you know how quickly it can ruin a good day (or night). As someone who’s dealt with GERD, ulcers, and a hiatal hernia over the years, I can tell you firsthand—none of it is fun. There’s nothing quite like the burning sensation creeping up your chest after a meal, or that tight feeling in your throat when lying down. And let’s not even get started on those nights when you have to prop yourself up just to get a little sleep.
What many people don’t realize is that acid reflux isn’t just an occasional annoyance. For some, it’s a constant battle that affects daily life, from chest pains to trouble swallowing. Over time, if left untreated, it can even lead to more serious issues. In this article, I’ll break down the causes of acid reflux, dive into the deeper issues like nighttime reflux and chest pain, and offer a few solutions based on what’s worked for me and countless others.
So, let’s start by understanding the basics—what is acid reflux, and why does it happen?
What Is Acid Reflux and Why Does It Happen?
Acid reflux happens when stomach acid flows back into the esophagus, the tube connecting your throat to your stomach. Normally, a valve at the bottom of the esophagus called the lower esophageal sphincter (LES) prevents acid from moving back up, but when this valve weakens or relaxes inappropriately, acid escapes. The result? That burning sensation we all know as heartburn.
For some people, acid reflux is an occasional nuisance after eating too much or consuming certain trigger foods. But for others, it’s a daily struggle that leads to more severe symptoms and complications. When acid reflux becomes a chronic issue, it’s often diagnosed as Gastroesophageal Reflux Disease (GERD), which can have a significant impact on your quality of life.
I’ve dealt with GERD personally, and let me tell you, it’s more than just an uncomfortable feeling after meals. It can lead to long-term issues like erosion of the esophagus, difficulty swallowing, and even chest pain. But what triggers this painful condition? The causes of acid reflux vary from person to person, so let’s dive into some of the common and not-so-common reasons behind it.
Now that we understand what acid reflux is, let’s explore the common causes in more detail.
Common Causes of Acid Reflux
Acid reflux can be triggered by a variety of factors, and understanding what’s causing yours is the first step toward managing it. For many, it’s not just one thing but a combination of lifestyle habits, foods, and even physical conditions that lead to the dreaded burn. Here’s a closer look at some of the most common causes of acid reflux:
1. Overeating
One of the biggest culprits of acid reflux is simply eating too much. When your stomach is overly full, it puts pressure on the LES, making it easier for acid to escape into your esophagus. This is why you might notice symptoms more often after a large meal, especially if you’re lying down right after eating.
2. Spicy and Acidic Foods
I’ve learned the hard way that certain foods are almost guaranteed to trigger acid reflux. Spicy dishes, tomatoes, citrus fruits, and foods high in acidity (like coffee) can irritate the lining of your esophagus, leading to more frequent reflux episodes. The more acidic the food, the more likely it is to cause trouble.
3. Alcohol and Smoking
Both alcohol and smoking weaken the LES, allowing acid to flow back up more easily. Alcohol can also irritate the stomach lining, making your symptoms worse. Cutting back on these can make a significant difference in how often you experience reflux.
4. Obesity
Carrying extra weight, especially around your abdomen, increases pressure on your stomach. This pressure can push acid up into the esophagus, causing reflux. Losing weight, even a small amount, can alleviate symptoms for many people.
5. Pregnancy
Pregnant women often deal with acid reflux, especially in the later stages when the baby is pressing on their stomach. Hormonal changes during pregnancy also relax the LES, making it easier for stomach acid to escape.
6. Medications
Certain medications, including anti-inflammatory drugs, blood pressure medications, and muscle relaxers, can weaken the LES or irritate the esophagus, leading to more frequent reflux.
7. Stress
Stress doesn’t directly cause acid reflux, but it can exacerbate symptoms. When you’re stressed, your body produces more stomach acid, which can trigger or worsen reflux.
These are some of the most common causes of acid reflux, but it’s important to remember that everyone’s triggers are different. If you’re looking for more insight into other stomach-related issues, check out this detailed article on lower left abdominal pain and when to worry.

Next, let’s talk about when acid reflux becomes a deeper issue and leads to more serious symptoms like chest pain and difficulty swallowing.

When Acid Reflux Becomes a Deeper Issue: Chest Pain, GERD, and More
For many, acid reflux is an occasional inconvenience, but when it becomes a regular part of your life, it can lead to more serious symptoms and complications. I know firsthand how frustrating it can be when it’s not just about the occasional heartburn but something deeper. Let’s look at some of the more troubling issues that can arise from chronic acid reflux.
1. Chest Pain
One of the scariest symptoms of acid reflux is chest pain, which can sometimes mimic the feeling of a heart attack. This pain occurs when stomach acid irritates the lining of the esophagus, leading to a burning sensation or sharp pain in the chest. If you experience chest pain frequently, it’s important to seek medical advice to rule out any cardiac issues.
2. Difficulty Swallowing (Dysphagia)
Chronic acid reflux can also cause scarring and narrowing of the esophagus over time, making it difficult to swallow. This condition is known as dysphagia and can become a serious issue if left untreated. You may notice a sensation of food getting “stuck” or feel like you need to swallow repeatedly to get food down.
3. Persistent Hoarseness or Sore Throat
If acid reflux reaches your throat or voice box, it can cause irritation and lead to symptoms like hoarseness, a sore throat, or even a chronic cough. For me, there have been times when I’ve woken up with a raspy voice, only to realize it’s because acid reflux had crept up during the night.
4. Nighttime Reflux and Sleep Issues
Nighttime reflux is a nightmare. Literally. Lying flat can make acid more likely to move up into your esophagus, and the result is waking up with burning pain, coughing, or even regurgitation. I’ve had nights where I had to sleep sitting up just to avoid these symptoms. Some people even experience a condition called sleep apnea, where their breathing stops momentarily during sleep due to acid irritating the throat and airway.
To make things even more frustrating, nighttime reflux can disrupt your sleep patterns, leaving you feeling exhausted during the day. If this sounds familiar, consider looking into natural remedies that may help ease symptoms at night, like the tips found in this home remedies for heartburn guide.
When acid reflux starts causing these deeper issues, it’s a clear sign that you need to take action. Let’s dive into how to deal with these more intense symptoms and explore treatments that can offer relief.

Dealing with Nighttime Reflux and Sleep Issues
Nighttime reflux can be one of the most frustrating symptoms of acid reflux, and I’ve had more than my fair share of sleepless nights because of it. If you’ve ever woken up in the middle of the night with a burning sensation creeping up your throat, you know how disruptive it can be. The problem is that lying down makes it easier for stomach acid to flow back into your esophagus, leading to those painful nighttime flare-ups.
1. Sleeping in an Upright Position
There have been plenty of nights where I had no choice but to sleep in a more upright position just to keep the acid at bay. Propping yourself up with pillows or using an adjustable bed can help keep the acid down where it belongs. It’s not the most comfortable solution, but it can make a big difference when it comes to getting through the night without waking up in pain.
2. Avoid Late-Night Meals
Another tip that helps reduce nighttime reflux is avoiding large meals—or even small snacks—before bed. From personal experience, I’ve found that cutting off food intake at least two to three hours before hitting the pillow is essential. Giving your stomach time to digest can significantly reduce the chances of acid creeping up while you sleep.
3. Raise the Head of Your Bed
If sleeping sitting up is too uncomfortable (which, let’s be honest, it often is), try raising the head of your bed. You don’t need to invest in an expensive adjustable bed—placing blocks or risers under the legs of your bed can work just as well. Elevating your upper body prevents gravity from pulling acid back into your esophagus.
4. Sleep on Your Left Side
Sleeping on your left side can help reduce reflux symptoms. Studies have shown that sleeping in this position can help keep stomach acid where it belongs, while sleeping on your right side can make symptoms worse. Whenever possible, I make an effort to sleep on my left side, and it’s helped keep the night-time flare-ups at bay.
Nighttime reflux isn’t just a minor annoyance—it can disrupt your sleep and take a toll on your overall well-being. If you’re struggling to get a good night’s rest because of reflux, try these tips and see what works best for you. You may also want to check out this quick fix for insomnia to ensure your sleep routine is set up for success, especially if nighttime reflux is a regular challenge.
Next, let’s explore some effective treatments and lifestyle changes that can help bring long-term relief from acid reflux.

Treatments: Lifestyle Changes and Medications
Managing acid reflux can feel like a never-ending battle, but with the right lifestyle changes and medications, you can find some relief. Over the years, I’ve tried a variety of strategies—some work, some don’t, but the key is consistency and finding what fits your routine and body. Here’s what I’ve learned through personal experience.
1. Lifestyle Changes
Making small adjustments to your daily habits can make a big difference in reducing acid reflux symptoms. Here are a few changes that have helped me:
- Smaller Meals: Overeating is one of the biggest triggers for acid reflux. I’ve found that eating smaller, more frequent meals throughout the day helps prevent that uncomfortable feeling of fullness and reduces the pressure on my stomach.
- Avoiding Trigger Foods: Foods like spicy dishes, caffeine, chocolate, and citrus can make reflux worse. Keeping a food journal to track what triggers your symptoms can be helpful in cutting back on the worst offenders.
- Staying Upright After Meals: One of the best tips I can offer is to avoid lying down right after eating. I try to stay upright for at least two to three hours after a meal, and it’s made a huge difference in keeping reflux at bay.
- Weight Management: For those carrying extra weight, especially around the midsection, losing even a small amount can ease pressure on the stomach and reduce reflux.
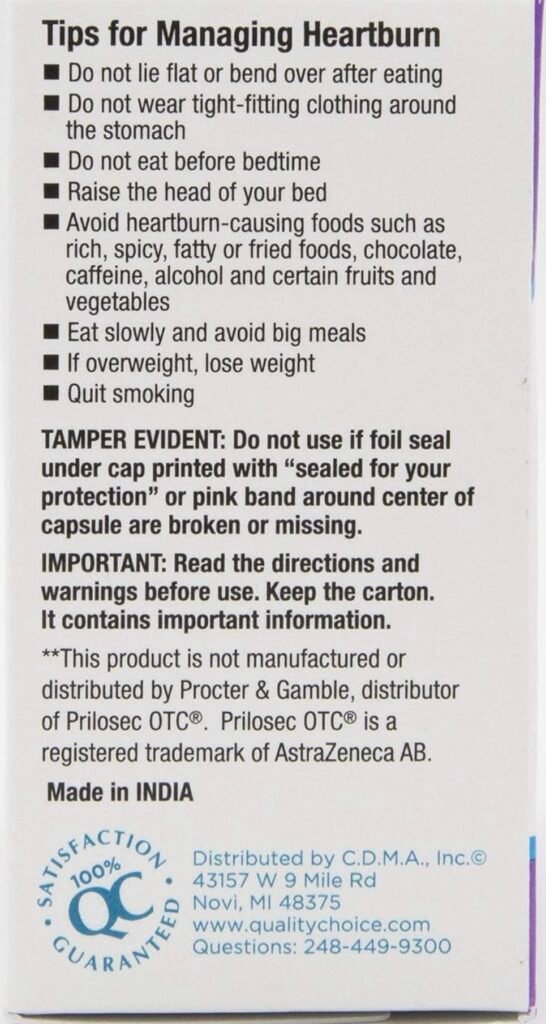
2. Over-the-Counter Medications
If lifestyle changes alone aren’t enough, medications can provide relief. I’ve tried several over-the-counter options, and the key is finding what works best for you. Here are a couple that have worked for me:
- Omeprazole Capsules: I’ve been taking Quality Choice Omeprazole in capsule form for years, and it’s been a game-changer for me. For some reason, the tablets just don’t seem to work as well, but the capsules provide consistent relief. It’s important to take them regularly, though, to maintain that protection against acid.
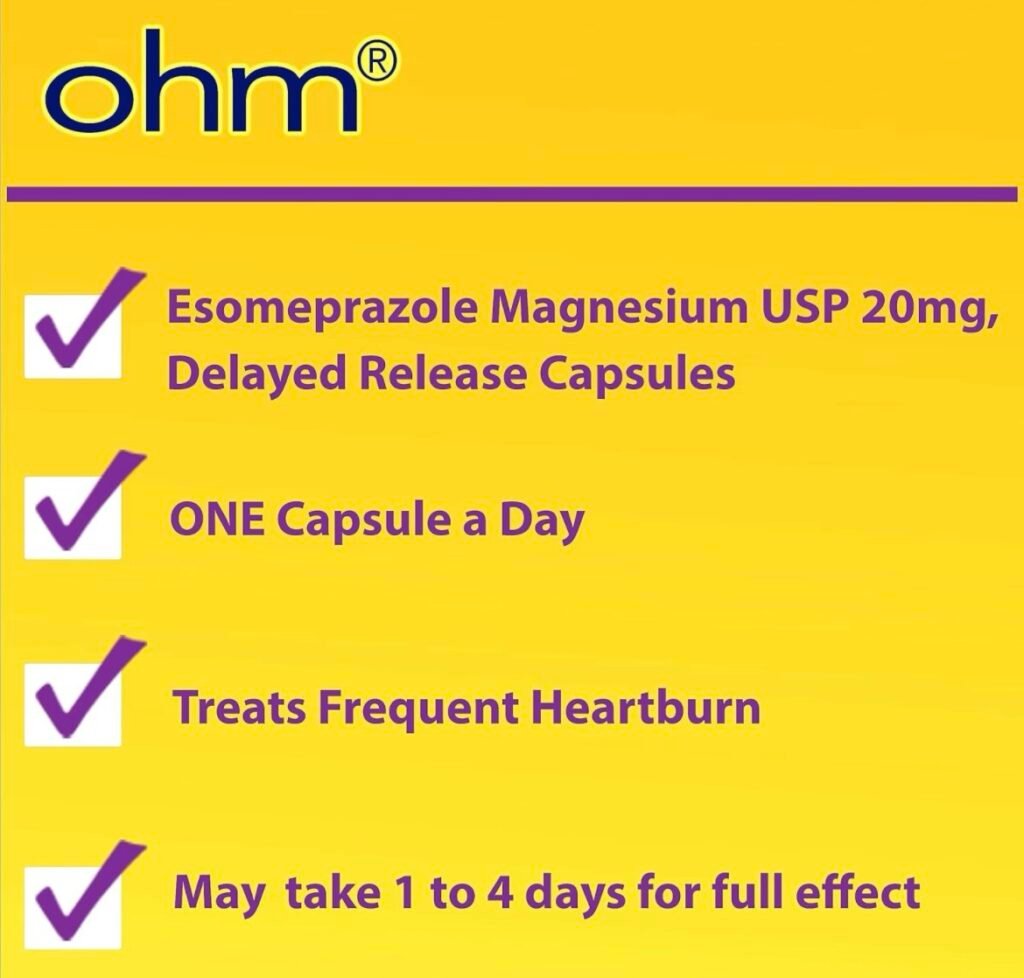
- Esomeprazole Magnesium (Nexium Alternative): If you’re looking for a more affordable version of Nexium, the OHM Esomeprazole Magnesium capsules are another option that has helped me manage frequent heartburn. Like Omeprazole, these capsules work by reducing the amount of acid your stomach produces, offering long-term relief.
3. Proton Pump Inhibitors (PPIs)
PPIs are a more long-term solution for those dealing with chronic acid reflux. These medications, like Omeprazole and Esomeprazole, reduce stomach acid production and are best used under the guidance of a doctor if you’re experiencing severe symptoms regularly. While they’re effective, they should be used cautiously and according to a doctor’s recommendation, as long-term use can come with side effects.
4. Natural Remedies
Sometimes, natural remedies can offer additional support for managing acid reflux. I’ve tried things like apple cider vinegar and ginger tea, and while they can help in mild cases, they’re no replacement for medications if you’re dealing with severe reflux. However, incorporating these into your routine may offer some extra relief alongside other treatments.
For more natural ways to address stomach issues, you can check out home remedies for heartburn and explore different solutions that might complement your existing treatments.
Next, we’ll discuss when acid reflux becomes serious and how to know when it’s time to see a doctor for potential complications.

When to See a Doctor: Serious Complications
While acid reflux can be managed with lifestyle changes and medications, it’s important to recognize when the condition is becoming more serious. For some people, chronic acid reflux can lead to complications that require medical intervention. I’ve had my own scares with more intense symptoms, and knowing when to consult a doctor made all the difference.
1. Barrett’s Esophagus
One of the long-term risks of untreated GERD is a condition called Barrett’s esophagus, where the tissue lining the esophagus changes due to constant exposure to stomach acid. This condition increases the risk of developing esophageal cancer. If you’ve been dealing with acid reflux for years and start experiencing difficulty swallowing or unexplained weight loss, it’s time to speak with your doctor. They may recommend an endoscopy to check for Barrett’s esophagus.
2. Esophageal Cancer
Though rare, chronic acid reflux can increase the risk of esophageal cancer. The ongoing irritation caused by stomach acid can damage the esophagus, potentially leading to cancerous changes. If you notice persistent chest pain, difficulty swallowing, or blood in your stool or vomit, these are red flags that you shouldn’t ignore.

3. Chest Pain and Heart Attack Symptoms
It’s important to remember that chest pain associated with acid reflux can sometimes mimic the symptoms of a heart attack. I’ve had moments where chest pain from reflux made me pause and wonder if something more serious was going on. If you experience sudden, severe chest pain—especially if it radiates to your arm, neck, or jaw—it’s crucial to seek emergency medical attention to rule out heart problems.
4. Difficulty Swallowing (Dysphagia)
If you begin experiencing consistent difficulty swallowing, or feel like food is getting stuck in your throat, this could be a sign that your esophagus is narrowing. This condition, known as dysphagia, can occur when acid reflux causes scar tissue to build up in the esophagus. A doctor can evaluate this condition and offer treatment options to prevent further complications.
5. Persistent Nighttime Symptoms
As mentioned earlier, nighttime reflux can cause severe disruptions to your sleep. If you find that even lifestyle changes and medications aren’t providing relief, it’s time to consult a doctor. Chronic nighttime reflux can also lead to sleep apnea and other sleep-related disorders, impacting your overall health.
If you’re unsure whether your symptoms are just reflux or something more serious, don’t hesitate to reach out to your healthcare provider. Catching potential complications early can prevent bigger health issues down the road.
For those curious about how long reflux symptoms last or seeking additional ways to manage them, take a look at this article on how long heartburn symptoms last to get a better understanding of what to expect.
Finding Relief and Managing Acid Reflux Long-Term
Living with acid reflux can feel like a constant battle, but the good news is that with the right treatment and lifestyle changes, you can take control and get your life back. Over the years, I’ve found that a combination of medication, diet adjustments, and simple habits like elevating the head of my bed has made a huge difference. But don’t just take my word for it—there are plenty of others who have found success with the same strategies.

For many, Proton Pump Inhibitors (PPIs) have been life-changing. These medications reduce the production of stomach acid, providing relief from the constant burn. Personally, I’ve relied on Quality Choice Omeprazole and OHM Esomeprazole Magnesium for years, and the capsules have made a world of difference. I know I’m not alone in this—here are a few testimonials from people who have experienced the same kind of relief:
John S.
“I was suffering from acid reflux almost daily. The burning in my chest and throat was unbearable, especially at night. After trying various remedies, I finally gave in and started using Omeprazole capsules. Within just a few days, the burning was gone, and for the first time in years, I was able to sleep through the night without having to sit up. This medication has completely changed my life.”
Jessica R.
“After struggling with heartburn for years, my doctor recommended Esomeprazole. I was hesitant to rely on a daily medication, but I couldn’t handle the constant discomfort anymore. Within a week of taking it, I noticed a huge difference. I no longer feel the need to reach for antacids after every meal, and my reflux is under control. I feel like I’ve got my life back.”
Mike B.
“I’ve had GERD for over a decade, and nothing seemed to work long-term. It wasn’t until I tried Omeprazole capsules that I finally got consistent relief. I can eat without worrying about chest pain or heartburn, and I can finally sleep through the night without acid creeping up. I can’t imagine life without it now.”
These real-life stories show just how impactful PPIs can be in managing acid reflux. They’re not a quick fix, but for many people dealing with chronic reflux, they offer a reliable, long-term solution.
If you’re suffering from acid reflux, it’s worth talking to your doctor about whether a PPI like Omeprazole or Esomeprazole might be the right solution for you. Remember, getting your reflux under control can significantly improve your quality of life, allowing you to enjoy meals, sleep soundly, and go about your day without the constant discomfort of heartburn.
For those of you looking to explore more options or understand what might be causing your symptoms, you can also dive into these helpful resources on related stomach issues: lower left abdominal pain and stomach problems that cause back pain.
With the right treatment, whether through lifestyle changes, medication, or both, you can take control of your acid reflux and live without the constant burden of heartburn.

As an Amazon Associate we earn from qualifying purchases through some links in our articles.