Living with IBS-D (Irritable Bowel Syndrome with Diarrhea) has been a challenging journey that has shaped much of my adult life. For over a decade, I’ve navigated the ups and downs of this often unpredictable condition, facing symptoms that range from mildly annoying to utterly disruptive. Living with IBS-D means adapting to frequent bathroom trips, managing dietary restrictions, and sometimes feeling like my stomach is controlling my life.
Before I turned 30, I had already undergone multiple endoscopies and colonoscopies, trying to pinpoint the root of my gastrointestinal troubles. The process was exhausting, both physically and mentally, but receiving a diagnosis was a pivotal moment that allowed me to start managing my symptoms more effectively.
The Challenges of Living with IBS-D
One of the most frustrating aspects of IBS-D is its inconsistency. I often find myself dealing with diarrhea and constipation at the same time, a combination that seems almost unbelievable until you’ve experienced it. Diarrhea, while inconvenient, is something I’ve learned to manage with relative ease. Constipation, on the other hand, brings a wave of nausea that I find difficult to tolerate.
To cope, I rely on a daily stool softener to maintain some semblance of regularity. For my GERD, which often accompanies my IBS-D, I’ve been taking Omeprazole for years. It’s a medication I can’t imagine living without, as it keeps my acid reflux at bay and helps me manage the constant battle with my digestive system.
Importance of Management
Through my personal experiences, I’ve learned that effective management of IBS-D is crucial to improving quality of life. This article aims to share insights and strategies for living with IBS-D, offering hope and practical solutions for those on a similar journey. Whether it’s identifying triggers, making dietary adjustments, or finding emotional support, understanding this condition is the first step toward taking control of your life.
Understanding IBS-D
Irritable Bowel Syndrome with Diarrhea (IBS-D) is a subtype of Irritable Bowel Syndrome characterized by chronic abdominal pain and frequent diarrhea. Living with IBS-D can be incredibly challenging due to its unpredictable nature and the discomfort it brings. It’s not just about physical symptoms; it affects every aspect of life, from meal planning to social activities.
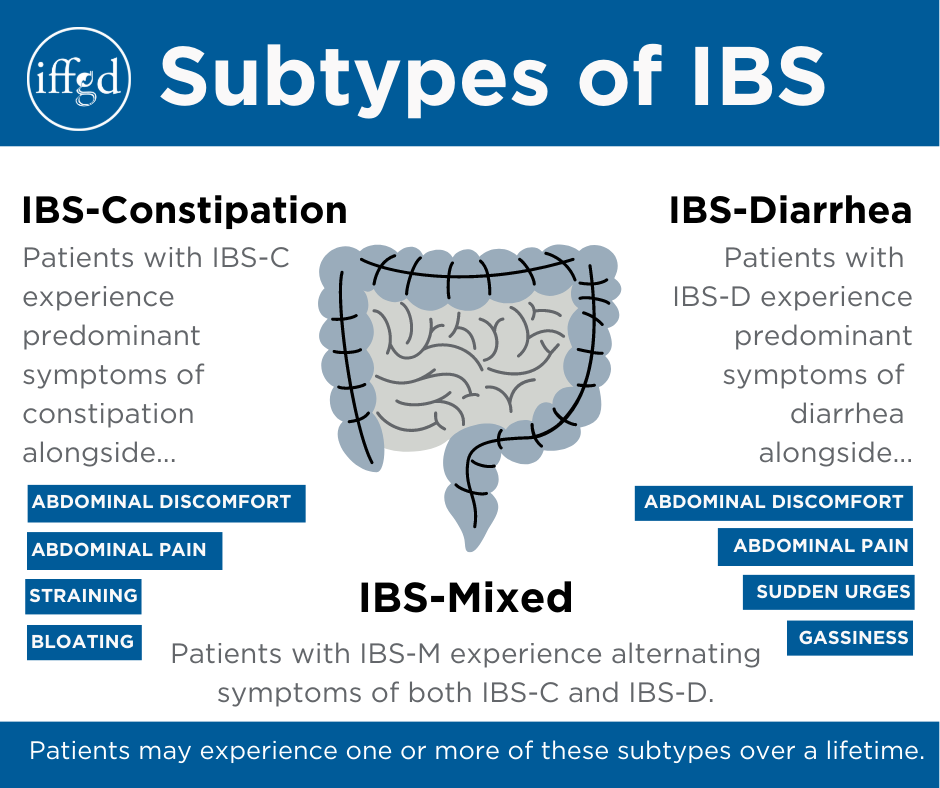
What is IBS-D, and How Does It Differ from Other Types of IBS?
IBS is a complex and often misunderstood condition. It can be categorized into three main types: IBS-C (constipation predominant), IBS-D (diarrhea predominant), and IBS-M (mixed, where symptoms alternate between constipation and diarrhea). Each type presents its own unique challenges.
IBS-D Specifics:
- Frequent Diarrhea: The hallmark of IBS-D is frequent, urgent bowel movements that can disrupt daily activities and lead to anxiety about being away from a bathroom.
- Abdominal Pain and Cramping: Often, the pain associated with IBS-D is severe and may feel like intense cramps or a dull ache. This pain is typically alleviated after a bowel movement.
- Bloating and Gas: Many people with IBS-D experience uncomfortable bloating and excessive gas, further contributing to the overall discomfort.
- Urgency: The need to rush to the bathroom can be embarrassing and stressful, especially in social situations.
My Diagnosis Journey
Before I received my diagnosis of IBS-D, my journey involved multiple medical tests and consultations. By the time I was 30, I had undergone three endoscopies and colonoscopies. While the procedures themselves were daunting, they provided valuable insights into my condition. Each test brought me closer to understanding what was happening in my body and how I could manage it more effectively.
Daily Struggles and Adaptations
One of the daily struggles of living with IBS-D is the unpredictability of symptoms. Some days are manageable, while others feel like a constant battle with my digestive system. Simple activities like eating out with friends or attending a meeting require careful planning and consideration of my symptoms.
I often experience a combination of diarrhea and constipation simultaneously, which seems counterintuitive but is a common occurrence with IBS-M. While diarrhea can be managed, constipation brings an intense nausea that can leave me feeling exhausted and frustrated.
Bathroom Access: Frequent trips to the bathroom are a norm, and I’ve learned to scout out restrooms wherever I go. Having a bidet has also become essential for comfort and hygiene, especially when facing multiple bathroom visits a day. If you’re interested in learning about the benefits of bidets, check out my article on why people choose to use a bidet.
Despite these challenges, I’ve found that understanding my condition and being proactive in managing symptoms makes a significant difference in my quality of life.
Common Triggers and Causes Of IBS
Living with IBS-D means navigating a complex web of potential triggers and causes that can exacerbate symptoms. Identifying and managing these triggers is crucial for reducing the frequency and severity of IBS flare-ups and improving overall quality of life.
What Causes IBS Flare-Ups?
IBS-D can be triggered by a variety of factors, including diet, stress, hormonal changes, and even certain medications. Understanding these triggers can help individuals develop a personalized plan to manage their condition effectively.
1. Dietary Triggers
Food is a major trigger for many people living with IBS-D. Certain foods can irritate the digestive system, leading to increased symptoms.
- Dairy Products: Lactose intolerance is common among people with IBS-D, making dairy a frequent culprit. Milk, cheese, and ice cream can all cause problems.
- Gluten: For some, gluten found in wheat, barley, and rye can trigger symptoms. While not everyone with IBS-D has celiac disease, gluten sensitivity is still a possibility.
- Fried and Fatty Foods: Foods high in fat can slow digestion, causing the stomach to produce more acid, which can worsen symptoms.
- Caffeine and Alcohol: Both can irritate the gut and increase symptoms of IBS-D, especially when consumed in large amounts.
- Spicy Foods: These can stimulate the digestive system and cause discomfort and diarrhea.
- High FODMAP Foods: FODMAPs are short-chain carbohydrates that can be poorly absorbed in the small intestine. Foods high in FODMAPs include certain fruits, vegetables, and artificial sweeteners.
Personal Experience: Over the years, I’ve identified that spicy foods and caffeine are significant triggers for me. Learning to avoid them has been a journey of trial and error, but it’s a key part of managing my IBS-D.
2. Stress and Emotional Triggers
Stress plays a significant role in triggering IBS-D symptoms. The gut is sensitive to stress and emotions, which can lead to increased motility and diarrhea.
- Work Stress: Deadlines and high-pressure work environments can exacerbate symptoms.
- Emotional Stress: Anxiety and depression can worsen IBS-D symptoms, creating a cycle of stress and digestive discomfort.
Personal Experience: I’ve noticed that during particularly stressful times, my symptoms tend to flare up. Managing stress through relaxation techniques like meditation and yoga has been beneficial in controlling these flare-ups.
3. Hormonal Changes
Hormones can affect the digestive system, and many women find that their symptoms worsen during their menstrual cycle due to hormonal fluctuations.
Personal Experience: Hormonal changes around my menstrual cycle often intensify my symptoms, making it essential to be extra cautious with my diet and stress levels during this time.

The Unpredictability of IBS-D
The unpredictability of IBS-D means that even minor changes in routine or diet can lead to a flare-up. Understanding these triggers has helped me minimize their impact, but it remains a daily challenge.
Identifying Personal Triggers
Identifying personal triggers requires careful observation and sometimes keeping a food and symptom diary. Recording what you eat and how you feel afterward can reveal patterns and help you avoid foods or situations that exacerbate your symptoms.
For those looking to understand more about stomach health and possible solutions, explore this comprehensive guide to stomach health.

Coping Strategies and Lifestyle Changes
Living with IBS-D requires a proactive approach to managing symptoms through strategic lifestyle changes and coping strategies. While medications and treatments are essential, personal habits and dietary choices play a significant role in controlling IBS-D symptoms. Here, I’ll share the strategies and lifestyle adjustments that have worked for me, making daily life more manageable and less stressful.
Dietary Changes for Living with IBS-D
Adopting the right dietary habits is crucial in managing IBS-D. Although it can be a bit of trial and error, finding the best foods for your digestive system can make a world of difference.
1. Following a Low FODMAP Diet
One of the most effective dietary strategies for many people with IBS-D is the low FODMAP diet. This approach involves eliminating foods high in fermentable carbohydrates that can trigger symptoms.
- What to Avoid: Foods like garlic, onions, wheat, certain dairy products, and artificial sweeteners.
- What to Include: Foods like bananas, blueberries, carrots, potatoes, and rice that are easier on the gut.
Personal Experience: When I first started the low FODMAP diet, I was surprised by how quickly my symptoms improved. By identifying and eliminating high FODMAP foods, I gained more control over my digestion.
2. Eating Smaller, Frequent Meals
Instead of having three large meals, I find it helpful to eat smaller, more frequent meals throughout the day. This approach helps to reduce the burden on the digestive system and prevents sudden flare-ups.
3. Staying Hydrated
Drinking plenty of water is essential for maintaining healthy digestion. It’s especially important when experiencing diarrhea, as dehydration can quickly become a concern.
Tip: Avoid caffeinated and sugary drinks, as they can exacerbate symptoms.
Stress Management Techniques
Stress is a major trigger for IBS-D symptoms, and managing it is crucial for symptom control. Here are some strategies that have worked for me:
1. Meditation and Mindfulness
Practicing mindfulness and meditation helps me manage stress and focus on the present moment. These techniques can reduce anxiety and have a calming effect on the digestive system.
2. Yoga and Exercise
Engaging in regular exercise, like yoga or gentle stretching, helps relieve tension and promote overall well-being. Physical activity stimulates digestion and reduces stress hormones.
3. Breathing Exercises
When stress levels rise, simple breathing exercises can provide immediate relief. Deep breathing helps activate the body’s relaxation response, which can alleviate IBS-D symptoms.
Personal Experience: Incorporating a daily routine of yoga and meditation has significantly reduced the frequency of my IBS flare-ups. It’s become an essential part of my daily routine, providing both physical and mental benefits.
How to Prevent IBS Flare-Ups
Preventing IBS-D flare-ups involves being mindful of triggers and making consistent lifestyle choices that support digestive health. Here are a few tips that have helped me manage symptoms:
- Identify Triggers: Keep a food diary to track what you eat and how it affects your symptoms. This will help you identify foods and situations that trigger flare-ups.
- Plan Ahead: Whether it’s meal prep or planning for a trip, being prepared can prevent stress-induced symptoms.
- Routine: Maintaining a consistent daily routine for meals and exercise helps keep my symptoms in check.
- Listen to Your Body: Pay attention to how your body reacts to certain foods and stressors, and adjust accordingly.
For those who experience heartburn alongside IBS-D, consider checking out these home remedies for heartburn that might complement your IBS management strategy.

Treatment Options for IBS-D
While lifestyle changes and home remedies play a significant role in managing IBS-D, there are also various treatment options available that can provide additional relief. These include medications, supplements, and natural remedies that can help control symptoms and improve quality of life.
Medications for IBS-D
Several medications are designed to help manage the symptoms of IBS-D. It’s important to work with a healthcare provider to find the right medication, as each person’s response can vary.
1. Anti-Diarrheal Medications
Examples: Loperamide (Imodium)
- How They Work: These medications slow down intestinal transit, reducing the frequency of bowel movements and helping to control diarrhea.
- Personal Experience: I occasionally use anti-diarrheal medications during particularly bad flare-ups or when I know I’ll be in situations where bathroom access is limited. They can be a lifesaver when I need quick relief.
2. Antispasmodics
Examples: Dicyclomine (Bentyl), Hyoscyamine (Levsin)
- How They Work: Antispasmodics help reduce intestinal muscle spasms, alleviating cramping and pain associated with IBS-D.
- Personal Experience: I’ve found that antispasmodics are helpful in managing the abdominal pain and cramping that often accompany my IBS-D symptoms.
3. Bile Acid Sequestrants
Examples: Cholestyramine (Questran), Colesevelam (Welchol)
- How They Work: These medications bind bile acids in the intestine, which can help reduce diarrhea in some individuals with IBS-D.
- Personal Experience: I haven’t used bile acid sequestrants myself, but I’ve heard from others in the IBS community that they can be effective, particularly for those whose symptoms are triggered by bile acid malabsorption.
4. Antidepressants
Examples: Tricyclic antidepressants (Amitriptyline), SSRIs (Citalopram, Fluoxetine)
- How They Work: Low doses of certain antidepressants can help reduce IBS symptoms by altering gut-brain communication and providing pain relief.
- Personal Experience: While I haven’t needed to take antidepressants specifically for IBS-D, it’s comforting to know they are an option if stress and emotional triggers become more prominent.
Supplements and Natural Remedies
In addition to traditional medications, there are natural remedies and supplements that can offer relief from IBS-D symptoms.
1. Probiotics
Examples: Lactobacillus, Bifidobacterium
- How They Work: Probiotics help balance gut bacteria, which can improve digestion and reduce IBS-D symptoms.
- Personal Experience: Adding a probiotic supplement to my daily routine has been a game-changer. It helps stabilize my gut flora, which in turn reduces both diarrhea and bloating.
2. Peppermint Oil
- How It Works: Peppermint oil has antispasmodic properties that can relax the muscles in the GI tract, reducing pain and cramping.
- Personal Experience: I’ve found peppermint tea soothing, and peppermint oil capsules are a convenient way to incorporate this remedy into my regimen.
3. Fiber Supplements
Examples: Psyllium husk, Acacia fiber
- How They Work: Soluble fiber supplements can help bulk up stool and reduce diarrhea.
- Personal Experience: Finding the right balance with fiber is crucial. Too much can worsen symptoms, but the right amount helps regulate bowel movements and prevent flare-ups.
4. Herbal Remedies
- Examples: Ginger, turmeric, chamomile
- How They Work: Herbal remedies can provide anti-inflammatory and soothing effects on the digestive system.
- Personal Experience: Herbal teas have become a part of my daily routine, offering both relief and comfort. Chamomile and ginger teas are my go-to choices for soothing an upset stomach.
Exploring Alternative Therapies
Some people find relief through alternative therapies, such as acupuncture, yoga, or cognitive-behavioral therapy (CBT). These approaches focus on the mind-body connection and can be effective in managing stress-related symptoms.
Personal Experience: Incorporating yoga and mindfulness practices has been incredibly beneficial for my IBS-D management. These activities help me maintain a calm mindset and reduce stress, which significantly impacts my symptoms.

Living with IBS and Diarrhea
Living with IBS-D means navigating the challenges of frequent diarrhea and the impact it has on daily life. From ensuring access to bathrooms to managing personal hygiene, finding practical solutions can make a significant difference. Here’s a look at how I’ve learned to manage living with IBS-D and why certain tools, like a bidet, have become essential in my routine.
Daily Life with IBS-D
Frequent Bathroom Trips
One of the realities of living with IBS-D is the need for frequent bathroom visits. Some days, I find myself going multiple times in just a few hours, which can be both exhausting and disruptive. This has taught me to always plan ahead and be aware of my surroundings, especially when leaving home.
- Planning Ahead: Whether it’s knowing where restrooms are located when I’m out or ensuring I have access to a bathroom at work, planning is key. I’ve learned to keep a mental map of reliable restrooms in public places and to carry essentials like wipes and hand sanitizer.
- Being Prepared: I always have a “just-in-case” kit with me, which includes extra clothes, wipes, and any medications I might need. This kit gives me peace of mind, knowing I’m prepared for unexpected flare-ups.
Dealing with Flare-Ups
Flare-ups can happen unexpectedly, often triggered by stress or something I’ve eaten. When this happens, I try to stay calm and remember that I’ve been through it before and will get through it again.
- Staying Calm: Stress can exacerbate symptoms, so I practice deep breathing or mindfulness exercises when I feel overwhelmed. This helps reduce anxiety and keeps me focused on managing the situation effectively.
- Dietary Adjustments: If a particular food has triggered a flare-up, I adjust my diet accordingly, eliminating the suspected culprit and focusing on gentle, gut-friendly foods.
My Experience with Bidets
With frequent bowel movements, maintaining hygiene is a top priority for me. A bidet has become an invaluable tool in my bathroom routine, offering both comfort and cleanliness.
Why Bidets Are Important for IBS Patients
- Improved Hygiene: A bidet provides a gentle and thorough cleanse, which is much more effective and comfortable than toilet paper alone. This is especially important when experiencing diarrhea, as wiping can cause irritation.
- Comfort: The soothing effect of water helps relieve any irritation caused by frequent wiping. For someone with IBS-D, this can make a huge difference in comfort throughout the day.
My Favorite Picks for Bidets
After trying various models, I’ve written an article on my favorite picks for bidets, which includes options that are easy to install and use. These bidets have transformed my daily routine, making it easier to manage my symptoms and maintain my comfort.
For anyone considering adding a bidet to their home, it’s a worthwhile investment that can greatly enhance personal hygiene and comfort. Learn more about why I think people choose to use a bidet and how it can make living with IBS-D more manageable.
Traveling with IBS and Diarrhea
Traveling presents unique challenges when you have IBS-D, but with careful planning and preparation, it can still be enjoyable.
Tips for Traveling with IBS-D
- Plan Your Meals: Research food options ahead of time to find places that offer IBS-friendly meals. If possible, bring safe snacks or meals with you.
- Know Your Route: Plan routes that include rest stops with accessible bathrooms. This can ease anxiety about not knowing when you’ll next have bathroom access.
- Stay Hydrated: Keep hydrated, but be mindful of your liquid intake before long trips to avoid unnecessary bathroom stops.
- Pack Essentials: In addition to my everyday kit, I make sure to have all necessary medications, extra clothes, and any specific foods or drinks that help manage symptoms during travel.
Personal Experience: Traveling with IBS-D used to fill me with dread, but over time, I’ve learned strategies to cope. Now, I focus on the joy of the journey rather than the fear of my symptoms. Being prepared and having a plan in place makes a significant difference.
Mental and Emotional Impact Of IBS
Living with IBS-D isn’t just a physical struggle; it has significant mental and emotional components as well. The unpredictability of symptoms, along with the physical discomfort, can take a toll on mental health, leading to feelings of anxiety, depression, and isolation. Here’s how I’ve navigated the emotional landscape of living with IBS-D and some coping strategies that have helped me manage these challenges.
How Living with IBS-D Affects Mental Health
Anxiety and Anticipation
One of the biggest emotional hurdles is the constant anticipation of symptoms. The fear of having an IBS flare-up in public or during important events can cause significant anxiety, affecting my daily life and social interactions.
- Social Anxiety: Worrying about bathroom accessibility or experiencing symptoms around others can lead to avoiding social gatherings or events. The fear of embarrassment is very real and often limits what I feel comfortable doing.
- Generalized Anxiety: The unpredictable nature of IBS-D symptoms creates a constant undercurrent of anxiety, impacting my ability to relax and enjoy life.
Depression and Isolation
The emotional burden of IBS-D can also lead to feelings of depression and isolation. When symptoms are severe, it’s easy to feel alone in the struggle, especially when others don’t fully understand the condition.
- Feeling Misunderstood: Many people don’t understand the complexities of IBS-D, leading to frustration when explaining why certain activities or foods are off-limits. This can create a sense of isolation.
- Mood Changes: Constant pain and discomfort can lead to mood swings, making it difficult to stay positive and engaged with life.
Impact on Self-Esteem
IBS-D can affect self-esteem, as managing symptoms can sometimes feel overwhelming and out of control. The constant worry about symptoms can lead to negative self-talk and a decrease in self-confidence.
Personal Experience: I’ve faced days where I felt overwhelmed by the weight of living with IBS-D. It’s challenging to remain optimistic when symptoms disrupt plans and affect my mood. Learning to manage these emotions is an ongoing process, but I’ve found strategies that help mitigate their impact.

Coping Strategies for Managing Emotional Challenges
Building a Support System
Having a support system of understanding friends, family, and healthcare professionals is crucial. Sharing experiences with others who have IBS-D can provide comfort and remind you that you’re not alone.
- Communication: Being open about my condition with those close to me has helped build understanding and empathy. It allows others to support me better and reduces feelings of isolation.
- Support Groups: Joining support groups or online communities can be incredibly beneficial. Hearing from others who experience the same challenges provides validation and new coping strategies.
Mindfulness and Stress Reduction
Incorporating mindfulness practices and stress reduction techniques has been vital in managing the mental health aspects of IBS-D.
- Mindfulness Meditation: Regular mindfulness meditation helps me stay present and reduces anxiety about future symptoms. It’s a practice that helps ground me and provides a sense of control.
- Yoga: Yoga combines physical movement with mindfulness, offering both physical relief and mental relaxation. It’s been an integral part of my routine, helping to alleviate stress and improve mood.
- Deep Breathing Exercises: Simple breathing exercises can provide immediate stress relief, especially during a flare-up or when anxiety peaks.
Cognitive-Behavioral Therapy (CBT)
CBT has been shown to help individuals with IBS by changing negative thought patterns and developing coping mechanisms.
- How It Works: CBT focuses on understanding how thoughts and emotions influence behaviors, providing strategies to manage anxiety and depression.
Personal Experience: Engaging in CBT helped me gain perspective on how IBS-D affects my thoughts and emotions. It’s been a valuable tool in building resilience and developing healthier coping strategies.
Emphasizing Self-Care
Prioritizing self-care is crucial for managing the mental and emotional aspects of IBS-D. This includes making time for activities that bring joy and relaxation, such as reading, hobbies, or spending time in nature.
- Listening to My Body: Understanding and respecting my body’s limits has been key to reducing stress and avoiding flare-ups.
- Practicing Self-Compassion: Learning to be kind to myself and accepting that I’m doing my best, even on tough days, has been transformative.
Personal Experience: Practicing self-compassion was challenging at first, but it’s made a significant difference in how I cope with IBS-D. Allowing myself to have bad days without judgment has been freeing and empowering.

Living with IBS-D is a challenging journey that affects both physical and mental well-being. From managing unpredictable symptoms to navigating social situations and maintaining mental health, the journey is filled with hurdles. However, with a combination of personal experience, medical guidance, and lifestyle adjustments, it’s possible to manage this condition and improve quality of life.
Key Takeaways
Understanding Your Triggers
Learning what triggers IBS-D symptoms is a crucial step in managing them. By identifying specific foods, stressors, and situations that exacerbate symptoms, you can take proactive measures to avoid or minimize them. Keeping a food and symptom diary can be invaluable in pinpointing these triggers.
Coping Strategies
Implementing coping strategies like mindfulness meditation, yoga, and cognitive-behavioral therapy can help manage the mental and emotional impact of IBS-D. These techniques can reduce anxiety, improve mood, and enhance overall well-being.
Lifestyle Changes
Adopting dietary changes, staying hydrated, and maintaining a regular exercise routine are vital components of managing IBS-D. A low FODMAP diet and other tailored nutritional plans can help control symptoms, while regular exercise aids digestion and reduces stress.
Utilizing Support Systems
Building a support network of family, friends, healthcare providers, and fellow IBS-D sufferers can provide encouragement and understanding. Sharing experiences and advice with others who face similar challenges fosters community and reduces feelings of isolation.
The Importance of Self-Care
Practicing self-care is essential in managing IBS-D. Listening to your body, setting realistic expectations, and prioritizing self-compassion are key aspects of maintaining a balanced and fulfilling life despite the challenges.
While living with IBS-D is undoubtedly challenging, it doesn’t have to define your life. By understanding your body, embracing effective coping strategies, and utilizing available resources, you can manage symptoms and lead a fulfilling life. Remember, it’s a journey of self-discovery and resilience, and every step you take toward managing IBS-D is a victory.
If you’re interested in learning more about maintaining stomach health, you can explore more in-depth information at TummyCure’s guide to stomach health.
Encouragement and Support
To everyone dealing with IBS-D, remember that you are not alone. It’s okay to have difficult days, and seeking help and support is a sign of strength. With determination and the right tools, you can navigate life with IBS-D and embrace the possibilities of a brighter, more comfortable future.
As an Amazon Associate we earn from qualifying purchases through some links in our articles.